HemAway
About Hemorrhoids
Hemorrhoids
Signs and Symptoms
Internal and external hemorrhoids manifest differently, however, many people have a combination of these two types. Rarely, more serious bleeding that leads to anemia occurs, and life-threatening bleeding is even rarer. Many people feel anxious when faced with this problem and often seek medical help only when the case advanced.
Hemorrhoids
External Hemorrhoids
Hemorrhoids
Internal Hemorrhoids
Hemorrhoids
Etiology
The exact cause of symptomatic hemorrhoids is unknown. Certain factors are thought to play a role, including irregular bowel movements (constipation or diarrhea), lack of exercise, nutritional factors (a diet low in fiber), increased intra-abdominal pressure (prolonged strain, ascites, intra-abdominal mass or pregnancy), genetics, lack of valves within the hemorrhoidal veins, as well as aging. Other factors believed to increase the risk are obesity, prolonged sitting, chronic cough, and pelvic floor dysfunction. However, there is little evidence for this connection.
During pregnancy, the pressure of the fetus on the abdomen and hormonal changes lead to an increase in hemorrhoidal vessels. Childbirth also leads to an increase in intra-abdominal pressure. Pregnant women rarely need surgery, as the symptoms usually go away after giving birth.
Hemorrhoids
Pathophysiology
Hemorrhoidal pads are part of the normal human anatomy and become a pathological disease only when abnormal changes occur on them. Three main pads are present in the normal anal canal. They are in the left side position and the front and rear position on the right. They are not made up of either arteries or veins but are made up of blood vessels called sinusoids, the connective tissue of smooth muscles. There is no muscle tissue in the walls of the sinusoids, as in the veins. This group of blood vessels is known as the hemorrhoidal plexus.
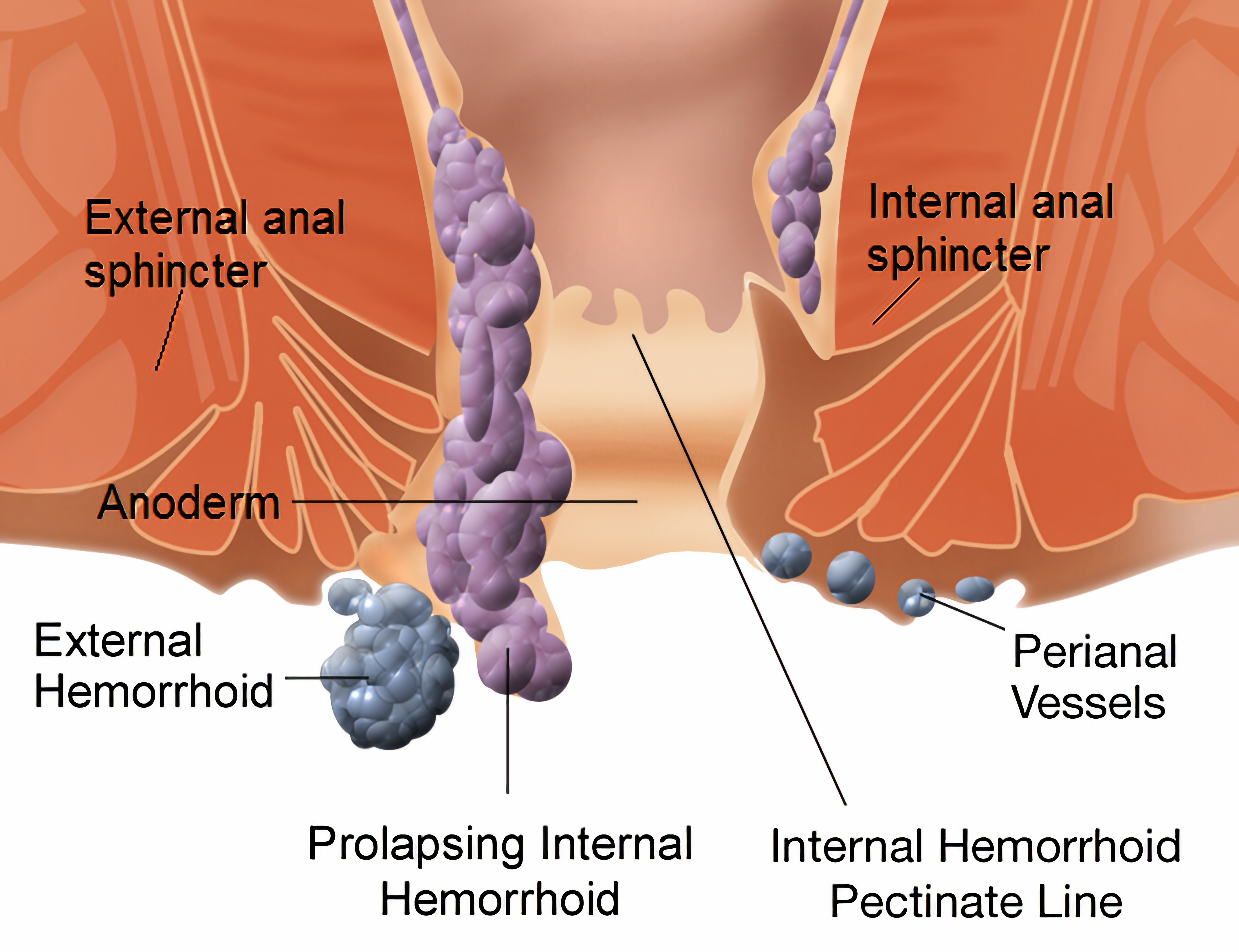
Hemorrhoidal pads are important for continence. They contribute 15-20% of the pressure of anal closure at rest and protect the muscles of the anal sphincter when passing excrement. When a person tenses, the intra-abdominal pressure increases, and the hemorrhoidal pads increase to help keep the anus closed. Hemorrhoid symptoms are believed to occur when these vascular structures slide downward or when venous pressure increases excessively. Increased anal sphincter pressure may also be among the symptoms of hemorrhoids. There are two types of hemorrhoids: internal from the upper hemorrhoidal plexus and external from the lower hemorrhoidal plexus. The jagged line divides these two regions.
Hemorrhoids
Division
Hemorrhoids can be external or internal. Internal ones occur near the beginning of the anal canal, and external ones at the anal opening… Internal hemorrhoids originate from the internal venous hemorrhoidal plexus in the upper part of the anal canal and the rectum. They enlarge, cover the skin-covered lower part of the anal canal and make the external hemorrhoidal venous plexus visible.
Hemorrhoids
Clinical picture
At the beginning and end of defecation, painless light red bleeding is possible, often in the form of running. There is blood on the excrement, it is not mixed with it. Hemorrhagic prolapse is common during defecation, which can become permanent. Hemorrhoids are generally not dangerous and do not endanger human life. The symptoms usually disappear within a few days. Symptoms of internal hemorrhoids are: excrement covered with light blood, blood on toilet paper or on a toilet bowl. However, internal hemorrhoids can come out of the anus and then they can be painful. Symptoms of external hemorrhoids include pain around the anus. The whole area around the anal opening is sensitive, painful and itchy.
Hemorrhoids
Diagnosis
Careful examination and correct diagnosis is important during any bleeding from the rectum or finding blood in the excrement. Bleeding can be a symptom of other diseases of the gastrointestinal tract, including colon tumors.
Rectal examination is often sufficient for diagnosis. Damaged blood vessels will be found in the area of the anus, and it is necessary for the doctor to perform a digitorectal examination (examination of the hindgut with a finger) looking for abnormalities.
Hemorrhoids are usually diagnosed by physical examination. Visual examination of the anus and surrounding area can diagnose external or prolapsed hemorrhoids.
Rectal examination is performed to detect possible rectal tumors, polyps, enlarged prostate, or abscesses. This examination is not possible without proper sedation due to pain, although most internal hemorrhoids are not associated with pain. Visual confirmation of internal hemorrhoids requires anoscopy, a hollow tubular instrument to which light is attached at one end. There are two types of hemorrhoids: external and internal. They differ in their position in relation to the toothed line. Some people may have symptoms of both types at the same time. If pain is present, it is more likely to be an anal fissure or external hemorrhoid than an internal hemorrhoid.
Hemorrhoids
Internal
- Grade I: No prolapse. Only blood vessels are conspicuous.
- Grade II: Tension prolapse that spontaneously decreases.
- Grade III: Tension prolapse requiring manual
reduction. - Grade IV: Prolapsed and cannot be reduced manually.
Hemorrhoids
External
External hemorrhoids are those that occur below the dentate or pectinial line. They are directly covered by the anoderm and distantly by the skin, both of which are sensitive to pain and temperature.
Hemorrhoids
Differential
Many anorectal problems, including fissures, fistulas, abscesses, colorectal cancer, rectal varices, and itching, have similar symptoms and can be misinterpreted as hemorrhoids. Rectal bleeding can also occur due to colorectal cancer, colitis, which includes inflammatory bowel disease, diverticular disease, and angiodysplasia.
If anemia is present, some other potential causes should be considered. Other conditions that lead to anal mass are skin growths, anal warts, rectal prolapse, polyps, and enlarged anal papillae. Anorectal varices due to increased portal hypertension (blood pressure in the portal pulmonary system) can manifest similarly to hemorrhoids but represent a different condition.
Hemorrhoids
Complications
Hemorrhoids
Prevention
Some preventative measures are recommended, including avoiding stress when trying to defecate, avoiding constipation and diarrhea, either by eating high-fiber foods and drinking plenty of fluids or by taking fiber as a supplement, as enough exercise. It is also recommended to spend less time in
try to defecate, avoid reading in the toilet, as well as weight loss in overweight people, and avoid lifting weights.
Hemorrhoids
Therapy
Mild cases of hemorrhoids can be treated by consuming more fluids and eating a high-fiber diet. Hemorrhoidal creams or suppositories can help reduce swelling and pain. It is useful to bathe in lukewarm water. Sometimes the condition is such that it requires surgery. Laser coagulation of hemorrhoids is increasingly used in treatment.
IMPORTANT: If you use HemAway you don’t need anything mentioned above
Hemorrhoids
Conservative
Conservative treatment mainly consists of a diet rich in fiber, consuming fluids orally to maintain hydration, using non-steroidal anti-inflammatory drugs (NSAIDs), sitting baths, and resting. Increased fiber intake has been shown to improve outcomes, and treatment success can be achieved with a variety of diets or the consumption of fiber supplements. However, there is no evidence that seat baths help during any time of treatment. If used, they should be limited to 15 minutes per session.
Hemorrhoids
Surgery
If conservative treatment and simple procedures fail, a large number of surgical techniques can be used. All surgeries are associated with some degree of complications including bleeding, infection, anal structures, and urinary retention, due to the close proximity of the rectum to the nerves that supply the bladder. There is also a small risk of fecal incontinence, especially fluid, with a reported rate between 0% and 28%. Mucosal ectropion is another condition that can occur after hemorrhoidectomy (often together with anal stenosis). This is when the mucous membrane of the anus is inverted from the anus, similar to a very moderate condition of rectal prolapse.
Excisional hemorrhoidectomy is the surgical removal of hemorrhoids that is used primarily only in serious cases. It is associated with severe postoperative pain, so it usually takes 2 to 4 weeks to recover. However, patients with third-degree hemorrhoids have longer-term benefits compared to rubber band ligation. This treatment is recommended for those with thrombosed external
hemorrhoids if performed within 24-72 hours. Glyceryl trinitrate ointment after the procedure helps to reduce both pain and faster healing.
Doppler-guided, transanal hemorrhoidal dearterialization is a minimally invasive treatment using ultrasound Doppler which precisely locates the inflow of arterial blood. The arteries are then ligated, and the prolapsed tissue is sutured back to its normal place. The recurrence rate of the disease is somewhat higher here, but there are fewer complications compared to a hemorrhoidectomy.
Separate hemorrhoidectomy, also known as separate hemorrhoidopexy, is a procedure that involves removing a large portion of abnormally enlarged hemorrhoidal tissue, followed by returning the remaining hemorrhoidal tissue to its normal anatomical position. This procedure is generally less painful and healing is longer compared to the complete removal of hemorrhoids. However, the chances of symptomatic hemorrhoids returning are higher than after conventional hemorrhoidectomy and are therefore generally recommended for second or third-degree disease.
Hemorrhoids
Epidemiology
Hemorrhoids are more common in the Caucasian type and in those with a higher socioeconomic status. Long-term outcomes are generally good although some people may have recurrent symptomatic episodes. Only a small percentage of people end up with surgery.
Hemorrhoids
History
You should give a recipe, a balm with a strong protective effect; acacia leaves, base crushed, and cooked together. Soak a strip of fine linen cloth and place it in the anus, until it recovers immediately.
In the works of Hippocrates from 460 BC. there is talk of a treatment that is similar to today’s bandaging of hemorrhoids with a rubber band:
“And hemorrhoids can be treated in a similar way by piercing them with a needle and tying them with a very thick woolen thread, and do not touch them until they fall off, and always leave one; and when the patient recovers, let him use helmets. ”
Hemorrhoids may also be described in the Bible.
Celsus (25 BC-14 AD) described the procedures of tying and cutting and considered possible complications. Galen advocated the view that the connection between the arteries and the veins should be separated, claiming that this would reduce both the pain and the spread of gangrene. Sushruta Samhita (4-5th century AD) is similar to Hippocrates’ words, but with an emphasis on the purity of the wound. In the 13th century, European surgeons such as Lafranc of Milan,
Guy de Scholiac, Henri de Mondville, and John Arden made great strides in the development of surgical techniques.
The word “hemorrhoid” first appeared in English in 1398, as a derivative of the old French emorroides, according to the Latin hæmorrhoida -ae, inherited from the Greek haimorrmhois “subject to bleeding”.
Hemorrhoids
NOTE:
the symptoms mentioned may not match your symptoms either.
The information of a medical nature that you can find on Wikipedia is, at best, general in nature and cannot replace the advice or diagnosis of a doctor or professional medical worker (cardiologist, dentist, nurse, midwife, pharmacist, etc.). Wikipedia is not a substitute for medical examination.
None of the individual article authors, database operators, developers, Wikipedia sponsors, or others associated with Wikipedia can be held responsible for the results or consequences of any attempt to apply or adapt any data you read in this encyclopedia.
None of what you may find on Wikipedia.org or any of the Wikimedia Foundation projects may be used to attempt to give or compose a medical opinion or diagnosis or otherwise interfere with a medical practice issue.